This is part 3, the last of a series of posts reflecting on some highlights in learning about movement that I experienced in this last year. In part 1, I addressed my experience with Applied Functional Science / Chain Reaction™ Biomechanics and presented an application of this approach using hip internal rotation. In part 2, I reflected my current thoughts on strength and conditioning. Now in part 3, I discuss my thoughts behind Fascia, Anatomy Trains, and Regional Interdependence.
Much of what we thought we knew about the biomechanical science of fascia and myofascial release is bunk. By saying this, I need to make it clear in advance that this does not change how we treat, rather it changes how we educate our patients and perhaps makes you think more critically about why you might, or might not, want to treat in a certain way. Greg Lehman provides an excellent review of fascial science on his blog.
So what about Anatomy Trains, which I have previously stated may be a beneficial overview for regional interdependence? As Dr. Lehman discussed, it is extremely unlikely that from a manual therapy standpoint we are making biomechanical changes to tissue. If anything, the biomechanical representation of Anatomy Trains better represents fascial adaptation to function and will only respond to progressive overload with daily stresses and exercise. Furthermore, if we look at function and movement, “Form Follows Function” , then the representation presented by Anatomy Trains may vary individually because tissue adapts to the stresses induced on a daily basis.
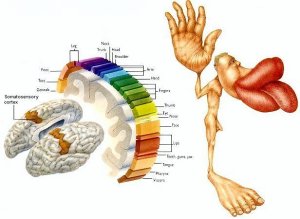
So we need to throw out the patterns presented by Thomas Meyers, correct? I personally do not think so. This is not the first time we have developed a general map which is not truly accurate of an individual representation. Our good friend the cortical homunculus also is an inaccurate representation of the somatosensory cortex.
Why? Because the brain is plastic and the somatosensory cortex adapts to how we interact with the world over time, which is most clearly demonstrated by cortical reorganization in phantom limb pain. Yet we still can use the homunculus as a general representation to give us a visual to for understanding sensation. Similarly, I still believe that seeing the patterns in Anatomy Trains can help us better see movement globally and therefore help guide treatment with complex patients representations. From a movement perspective, especially globally, we need to have some way to compartmentalize all the information and how they approximately relate to each other. Joint by joint osteokinematics and arthrokinematics help but can get complex quickly when you combine them with muscles and fascia. Patterns, such as those represented by Anatomy Trains, which encompass both bone and soft tissue, can help compartmentalize and make treatment more efficient if used appropriately. Of course, the reverse is also true, chasing patterns religiously will also take away from the most obvious, efficient, and appropriate treatment approach. Needless to say, these patterns do manifest themselves in our clients and patients from time to time, and to be ignorant of their general representations will cost you and your patient time.
As a side note, we are in a new era of our understanding of pain, with increasing emphasis on a neurophysiological role in this picture. There may be some overlap between the cortical homunculus and fascial adaptation over time. Since fascia is highly innervated with Ruffini and Pacini corpuscles, changes in fascia from physical adaptation to stress and from habituation to particular forms of movement may influence sensory perception and could theoretically be represented in the somatosensory cortex. With some recent evidence regarding the possible existence of a nocioceptive map which overlaps closely with the somatosensory cortex, there is the possibility that sensory rich fascia may be the interface that allows some of our voodoo with regional interdependence to occur, and why sometimes, specificity matters. This is purely hypothetical, but some ground work for the role of fascia and tendon pain (including pain referral) and their related cortical representation is discussed by Dr. William Gibson (His PhD thesis is available here: Pain sensitivity and referred pain in human tendon, fascia and muscle tissue.) But since we don’t have any other explanation for how manual therapy sometimes requires specificity and sometimes those points of specificity fall in the patterns represented by Anatomy Trains, this is where I am resting my patient education for the time being.
For a better summary than what I wrote above, I highly recommend a post by Alice Sanvito titled: “If we cannot Stretch Fascia, what are we doing?”.